Purpose
This report is a breakdown of goods and services performed by clinic any and all providers, also include cash sales.
Filter: Begin Date, End Date, Provider
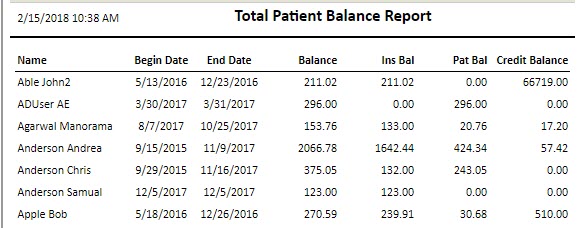
Header: Title, Date report was run
Column Data: Code, Description, Tax Amount, Amount, Units, Average
Patient payments: Taken in using Accept payment Tools, Total and amount applied
Payer Payments, checks, ins credit Cards, Direct Deposit. Totaled and listed by payer. Payments and adjustment totals.
Footer: Total AR Balance, Total Procedure Charges, Total Tax Amount, Take Backs, Total Cash, Total Co-Payment Amounts, Total Checks, Total Co-Payment Count, Total Checks Ins, Total Provider Reductions, Total Direct Deposit, Total Gross Sale, Total Discover, Total American Express, Total Visa, Total Master Card, Total Take Backs, Total Payments, Total Adjustments Minus, Total Adjustments Plus, Total Write Off, Total Collections, Total Adjustments, Total Adjustments + Payments