This task is to CHANGE or EDIT claims after submission to Insurance / Clearing House
NOTE: Claim Editing can be done to an original claim, once the original claim has been submitted to the payer. The Edited claim can be resubmitted electronically or a paper claim may be generated.
-
-
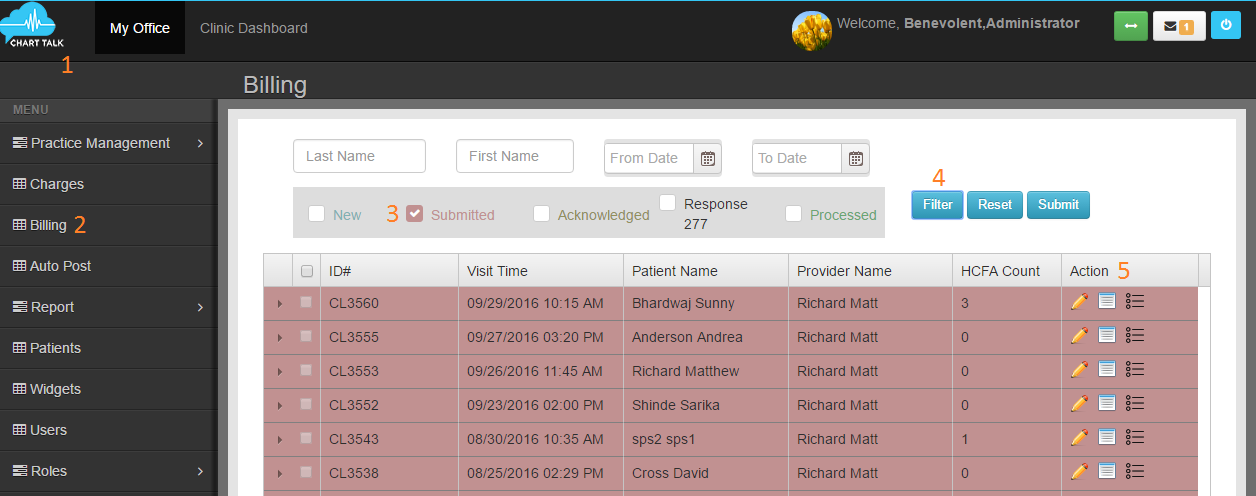
- Chart Talk Logo
- Billing
- Click ‘Submitted’
- Find the submitted claim you wish to correct/edit- you may filter by claim #, last name, first name and date
- Click ‘Loops’
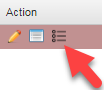
- Click ‘Pencil’
- Click ‘Create Corrected Claim’
- Update/correct the claim with the claim editing tool- make sure is default is checked. Note: if claim is not marked default will not update/submit to payer.
** IMPORTANT. You need to click on the CPT code from drop down after typing. The amount of the charge will auto populate. You will need to click the drop down to add modifiers if needed. Type in diagnosis pointers for each CPT code, if not already populated correctly.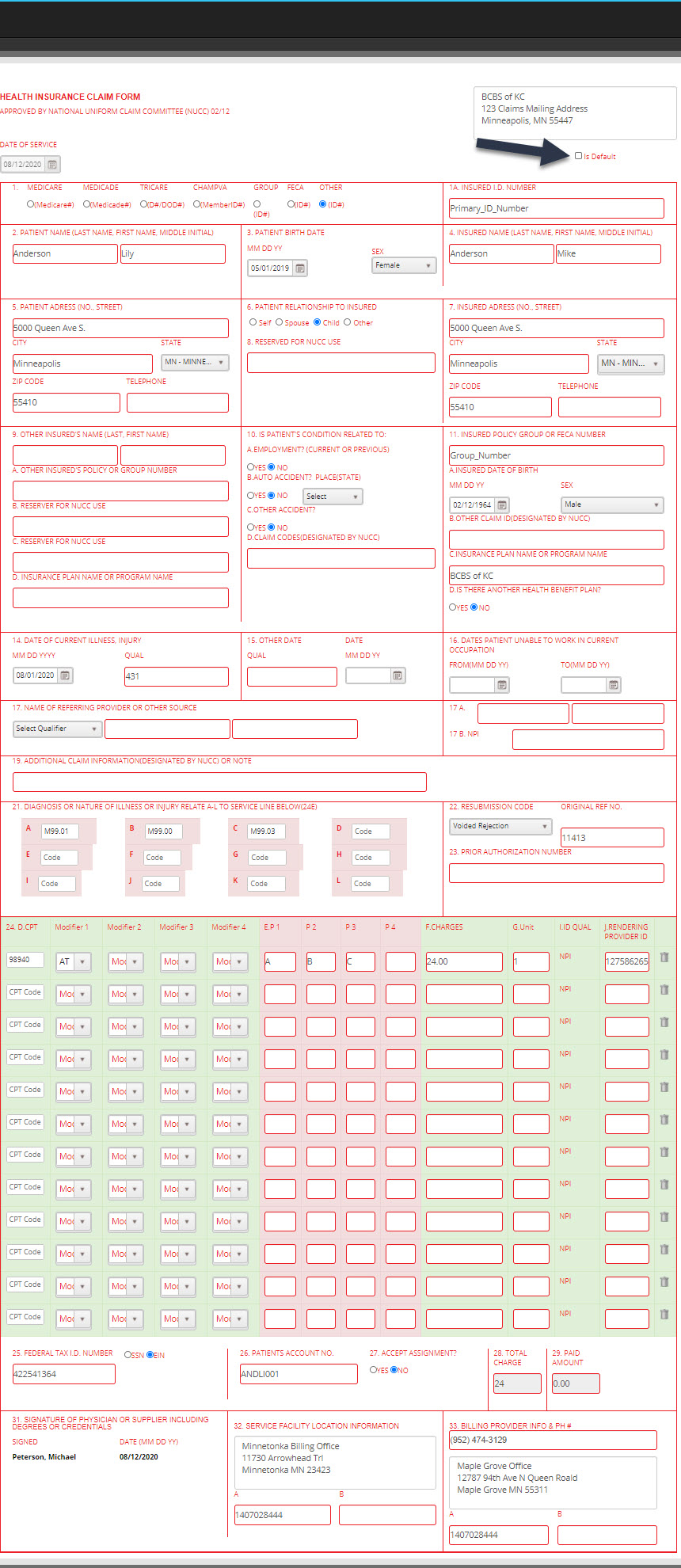
-
- Cleaninghouse Rejection(code:1 Original Claim)
- Payer Rejection (Code:7- Corrected Claim. Original Claim will be referenced in box 22)
- Voided Rejection (Code:8 Void Processed claim. Original claim will be reference in box 22)
- Electronic Claim- Submit to your clearinghouse electronically
- Download- Download as 837 text file
- Paper Claim- Generate paper claim to be printed
- Example: if you are submitting the same exact CPT codes on the new claim make sure you un check the originals to avoid any payments being put to the original claim when they now should go onto the edited claim.
NOTE: if there is payment applied to a CPT code it will need to be detached before it can be de-selected from the manage charges list.**There are many reasons a claim may need to be edited and resubmitted ranging from errors to forgotten information. Each time a claim is edited, a history of that edit and re-submission is captured in the Claim History Tab. This tab will show the date of re-submission along with the notes you have created explaining the reason (notes field) for the re-submission.
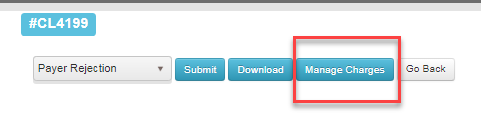
Before clicking update, you will need to select rejection reason. (located box 22)
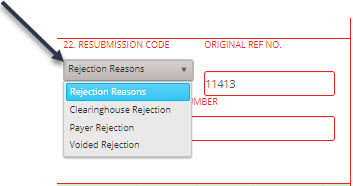
Rejection Reason
Select option for how to generate claim.
The next steps is to decide what you would like to show in Manage Payments for that date of service.
Click Manage Charges.
De-select and select items you would like to show in patients Manage Payments screen from the original claim.
IF you have NOT yet submitted the corrected claim electronically and DO NOT WANT TO: click download while in the billing screen. This will create an electronic file record within Chart Talk. Now follow the same directions above .