This task is to CHANGE or EDIT charges after it has been processed for billing but before it has been sent to the clearinghouse or payer.
- Chart Talk Logo
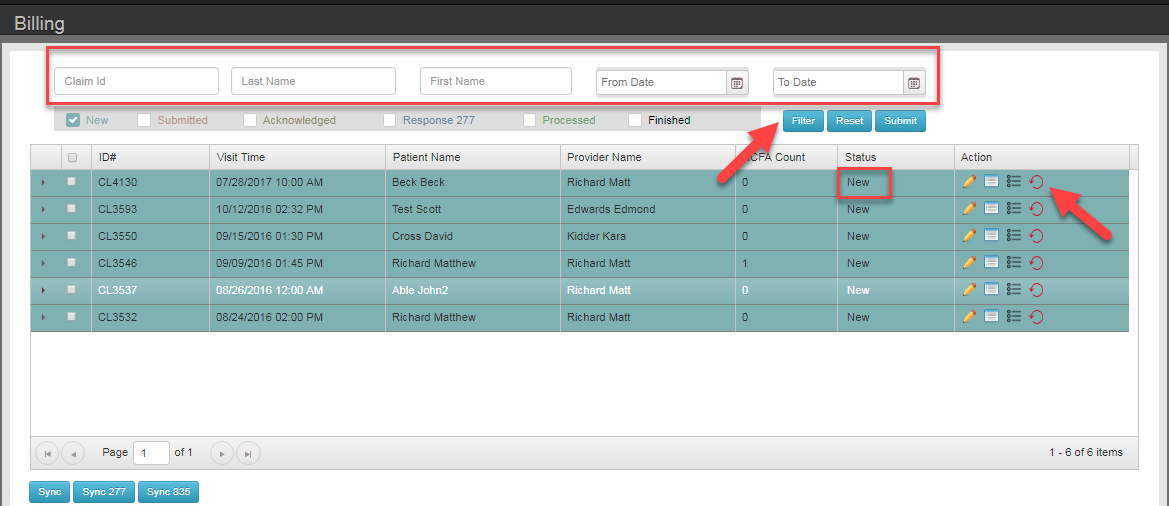
- Billing
- Find the patients date of service/claim you wish to reset back to the visit for edits. You may filter by claim #, Patient last name, first name a date range or click through pages
- Click the red circle with an arrow. This will reset the date of service back to the visit for edits to DX or CPT Codes
NOTE: must be in NEW status
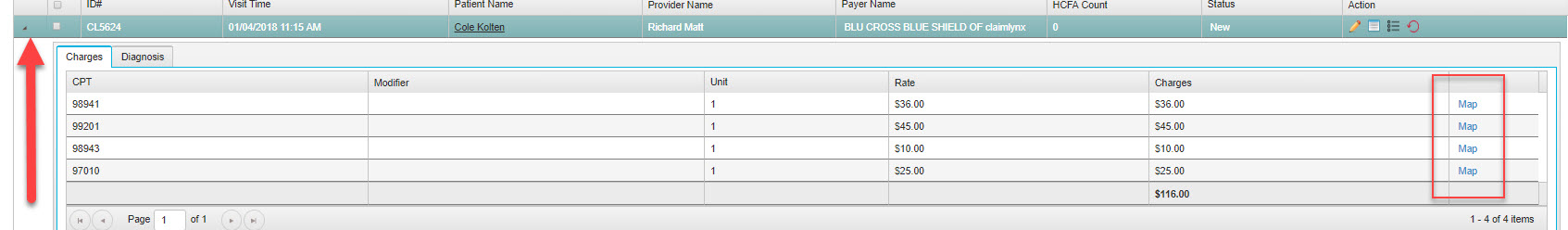
Edits that can be done in the billing screen: fee changes, mapping /pointers, Adding/changing/deleting modifiers
NOTE: if there is payment attached to any CPT code it will need to be detached in patients manage payments first.
Clicking the pencil will allow you to add/delete/change modifiers ( do this before a claim is submitted) and change the rate that is on the claim and in Manage Payments for that date of service.
Expand the Charge to change diagnosis code mapping .
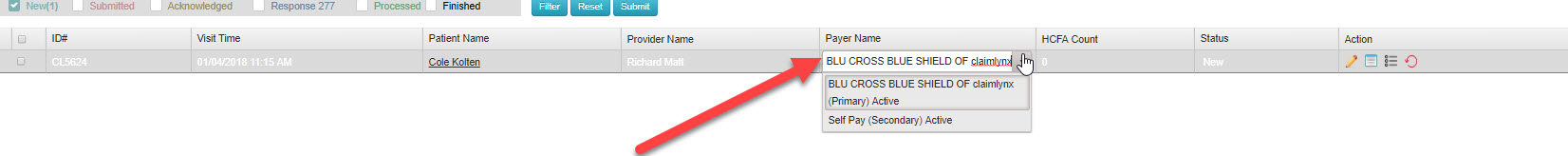
NOTE: To change a payer, select the payer column for the patient. A drop down will appear for active payers. NOTE: if selecting non-insured payer charge will move out of the billing screen to the non-insured charges screen.
REV20180919